Partnering together:
To support your work in bringing more appropriate patients to kidney transplantation before dialysis
Providing information and tools to support
kidney transplantation for appropriate patients
Access to renal replacement therapy can be multifaceted, including health care and financial considerations for patients, payers, and health care systems. Some of these considerations, outlined below, may help improve access to kidney transplant for appropriate patients.
Patients added to the waitlist before dialysis have over twice the living donor rate vs those added after dialysis.1
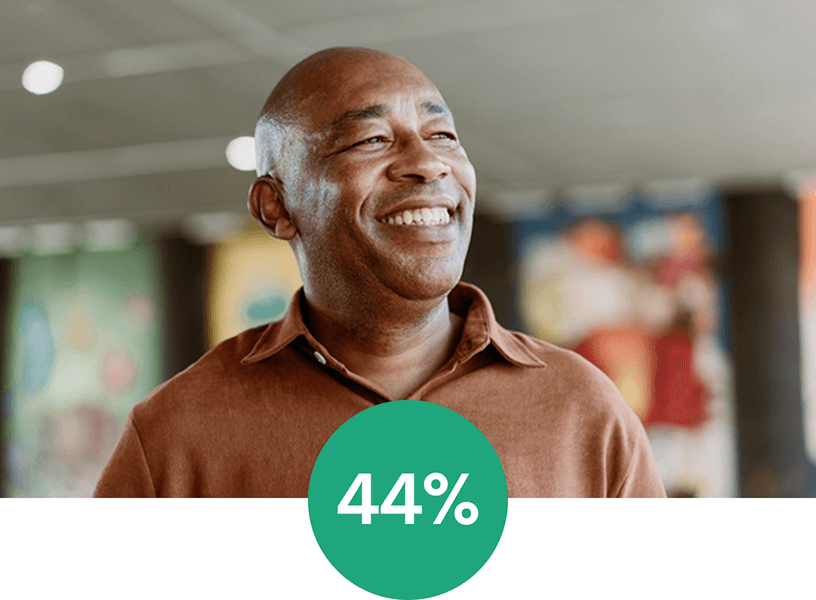
of patients wait-listed before dialysis received a living donor kidney transplant 3 years after the preemptive listing1,*
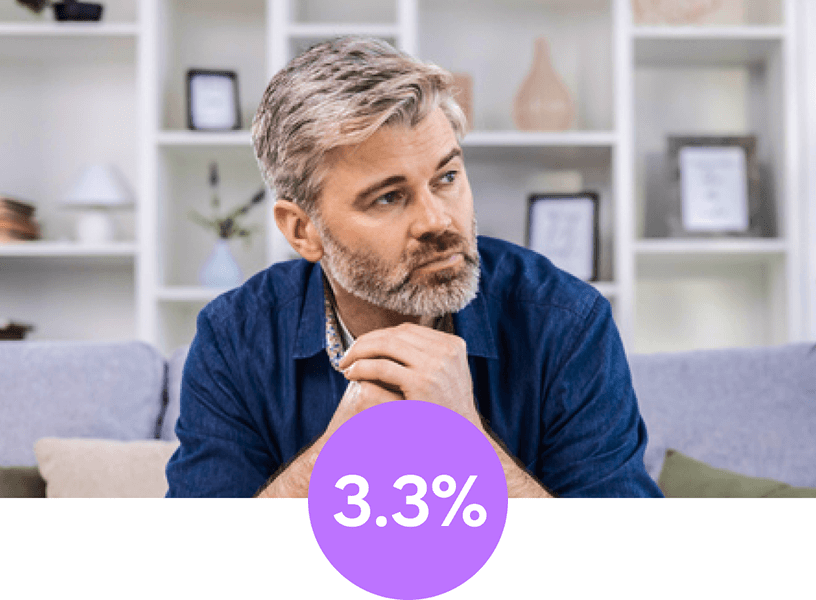
of Medicare Advantage beneficiaries with incident end-stage renal disease (ESRD) are waitlisted before initiating dialysis2,†
of US preemptive kidney transplants received a living donor vs 18% of patients after the start of dialysis in 2023.3‡
Put your patients with chronic kidney disease
(CKD) on the path to a pre-dialysis transplant.
Increasing access to pre-dialysis transplants may
benefit your transplant eligible beneficiaries2,4
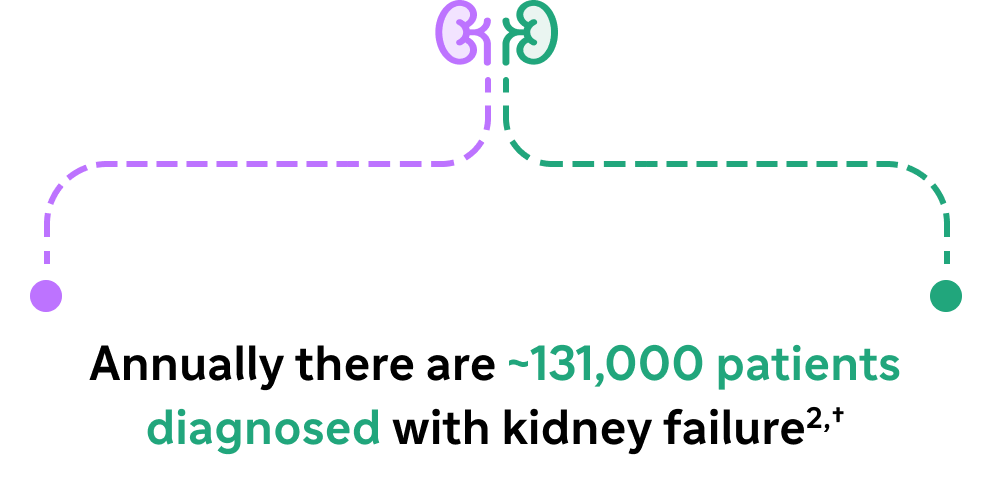
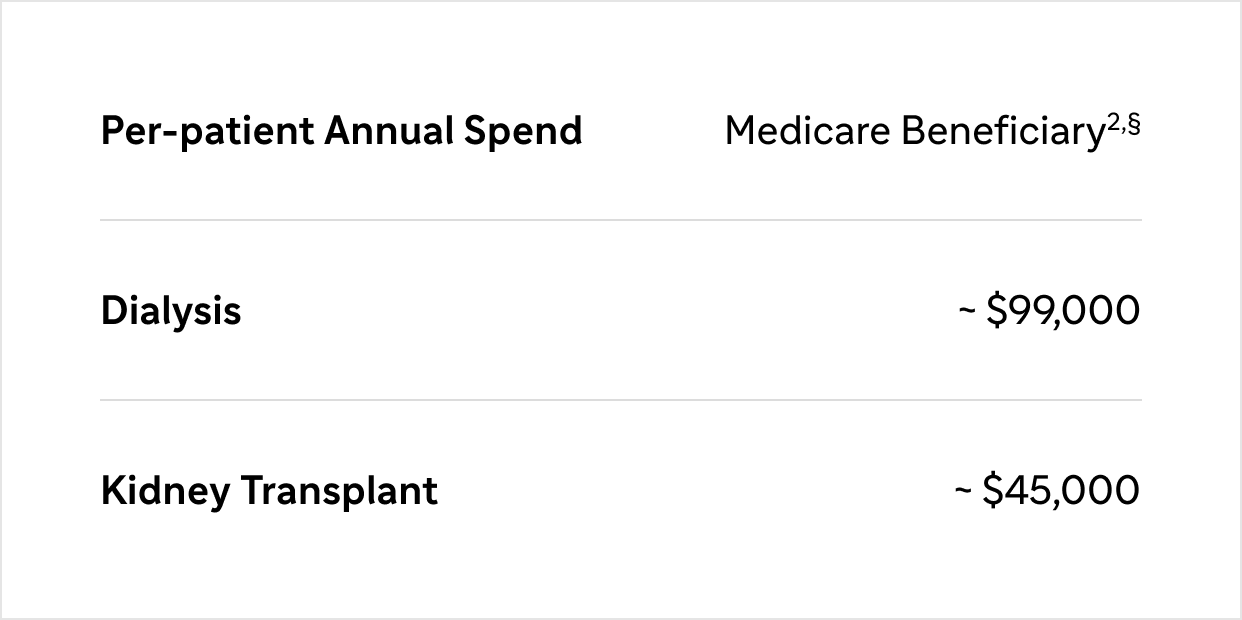
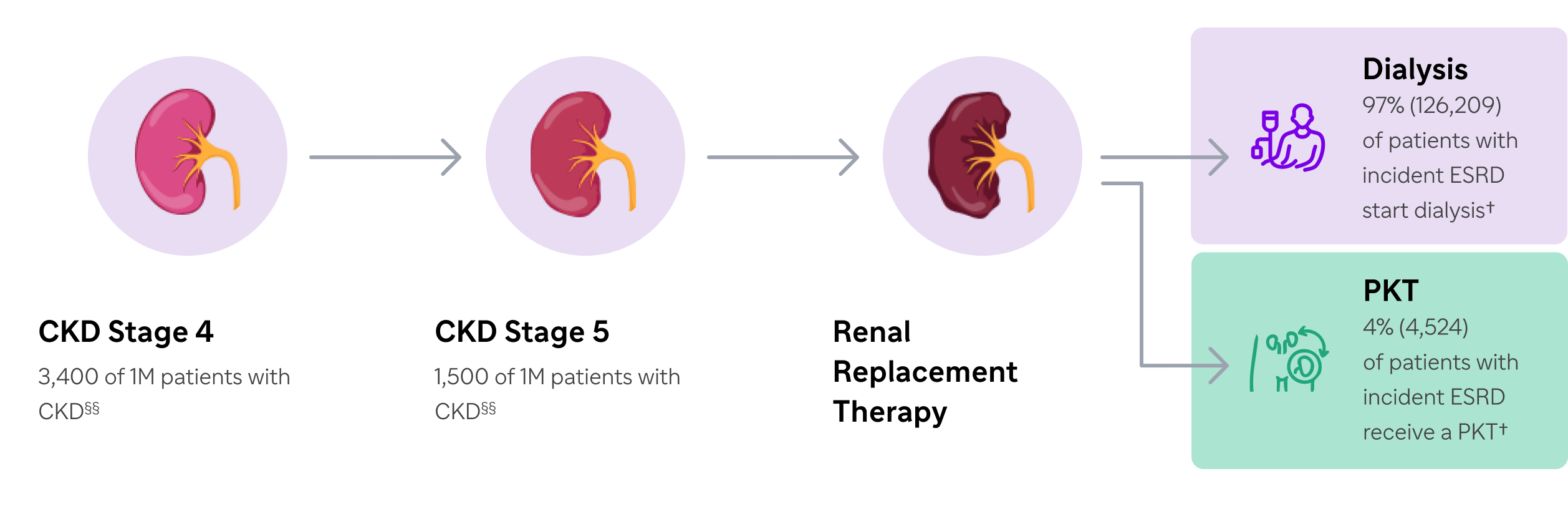
Dialysis
Most of these patients will follow a path that leads them to dialysis2,†
Kidney Transplant
Only ~4% (4,524) of patients will receive preemptive kidney transplant (PKT), the therapy recommended by Kidney Disease Improving Global Outcomes (KDIGO guideline)2,5,†
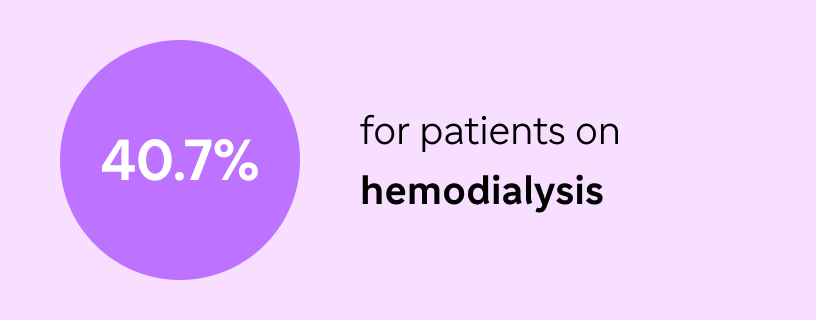
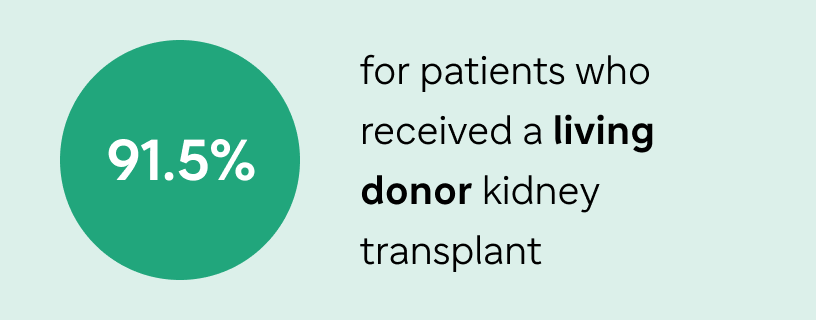
Based on data reported in 2018, adjusted 5-year survival for patients with ESRD was 2
For transplant eligible patients:
For appropriate patients:
Potentially eliminate or reduce medical spend for dialysis4
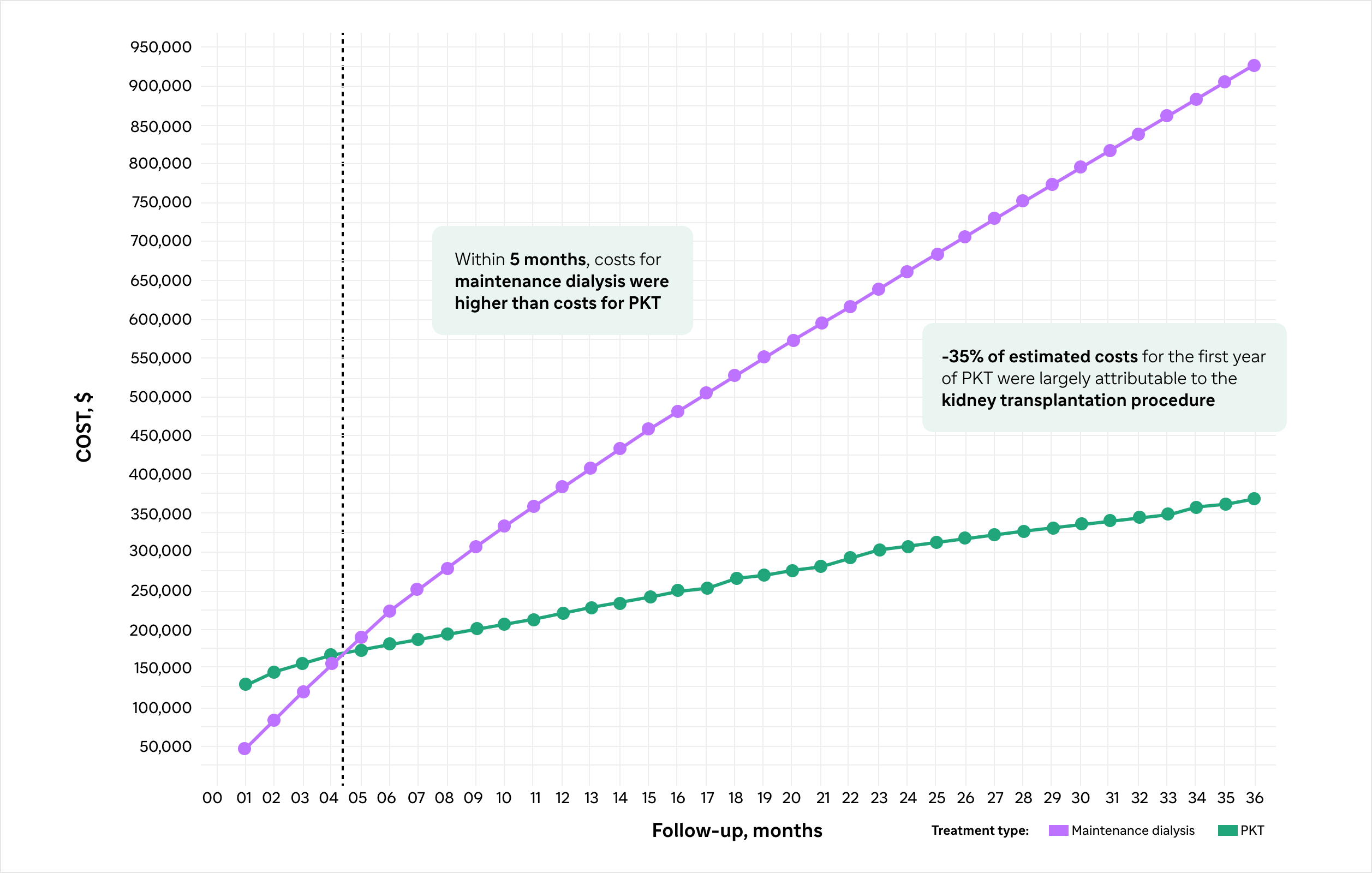
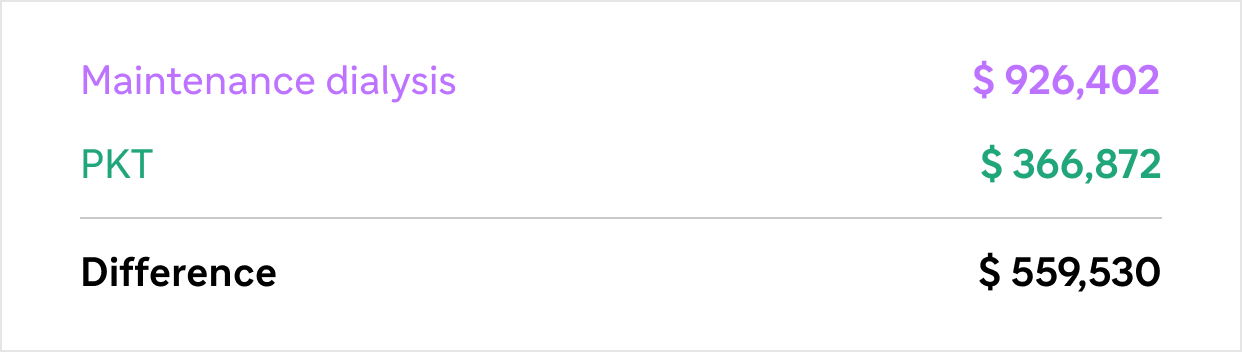
A study demonstrated that despite the initial high cost associated with kidney transplant, PKT in
appropriate patients may lead to lower health care costs over time compared to maintenance dialysis9,¶
Estimated All-Cause Cumulative Health Care Costs for Maintenance Dialysis or PKT in a
36-Month Period in Medicare Advantage and Commercial Insurance Enrollees 9,¶
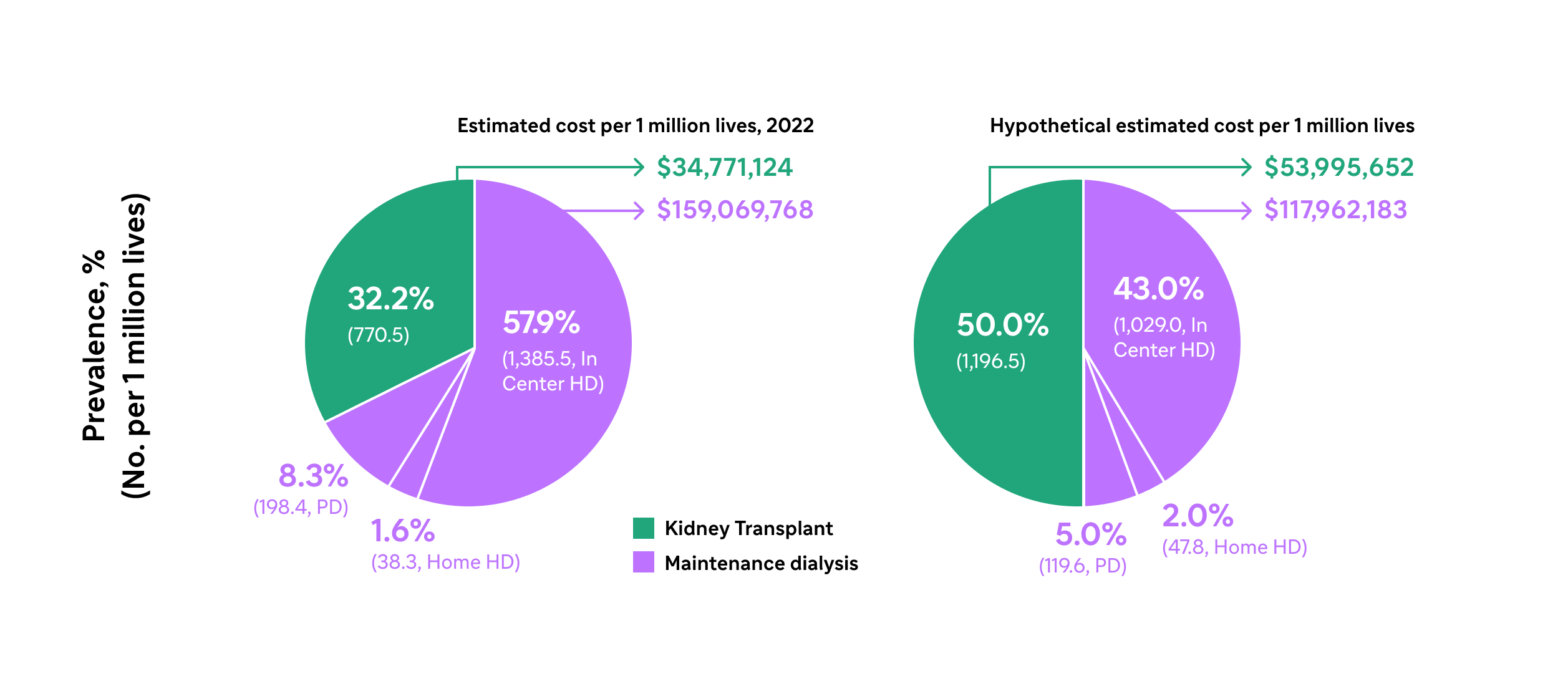
Increasing access to kidney transplantation in appropriate patients with ESRD may offer up to $21,883,057 per million lives in annual savings, based on a hypothetical scenario2,#
For appropriate patients:
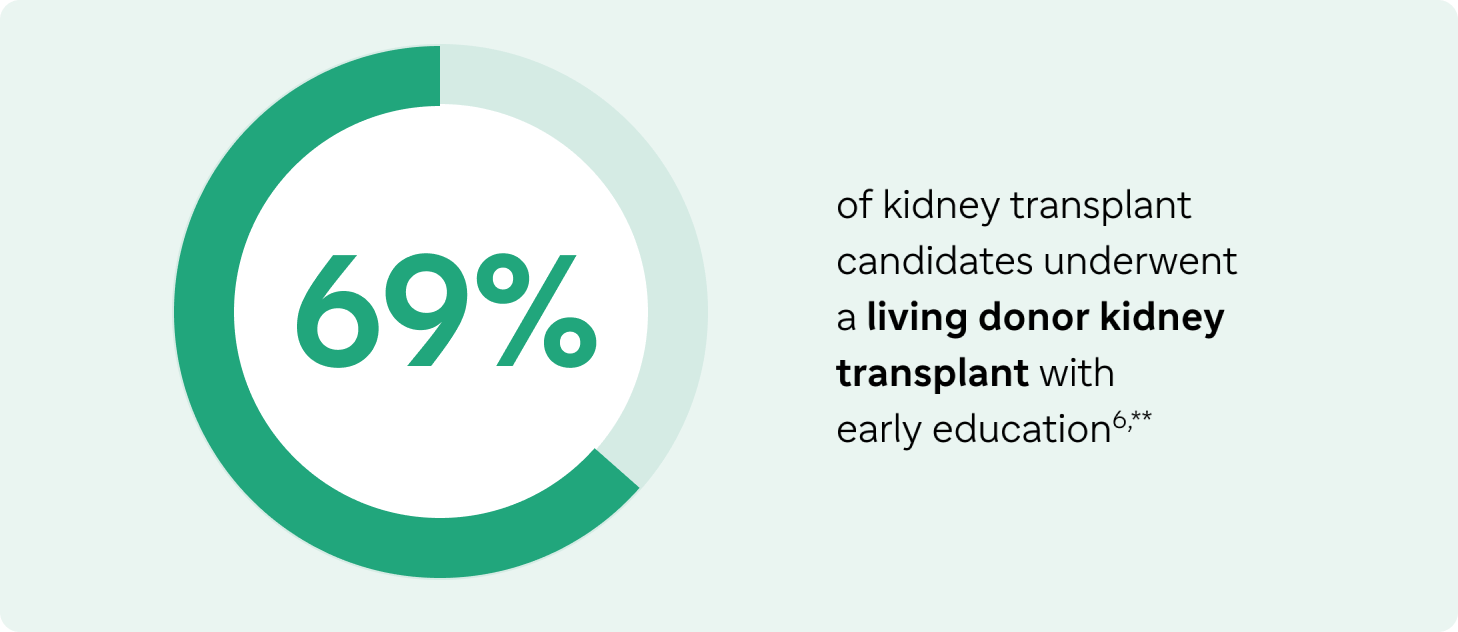
Increase living donor transplant rates by providing kidney disease education6
Only 5.6% of patients with incident ESRD were waitlisted before the initiation of dialysis2,‖
Early kidney disease education (KDE) (eg, at CKD stage 4) can lead to an increased use of living donor PKT6,**
A study evaluated kidney transplant outcomes associated with receipt of KDE among patients with ESRD9,††
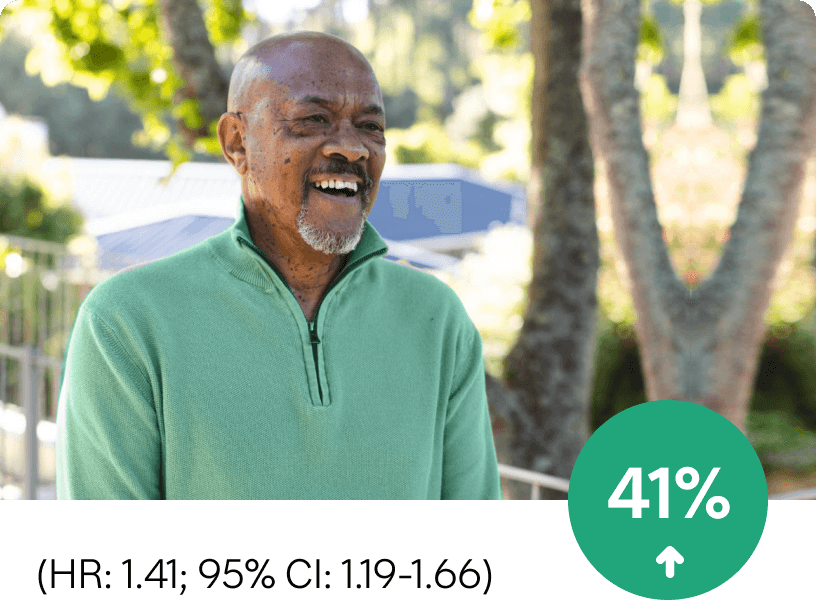
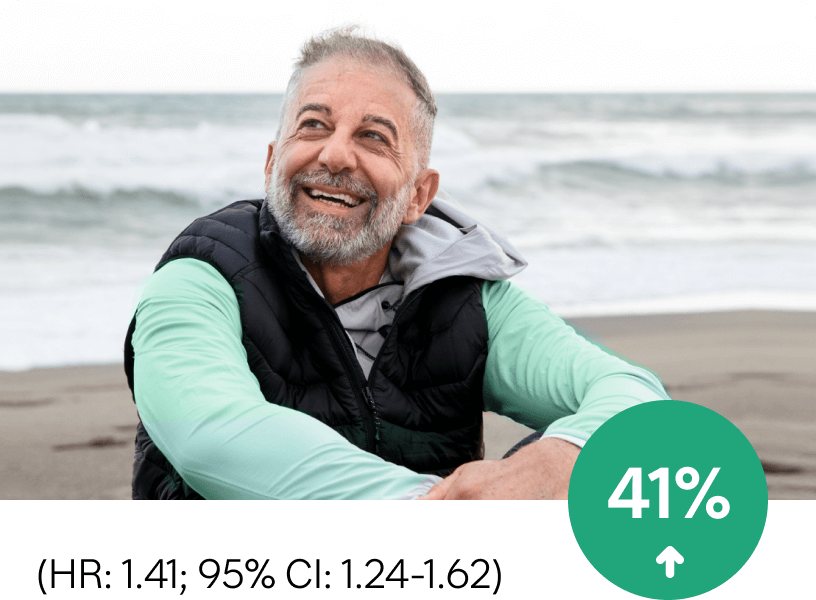
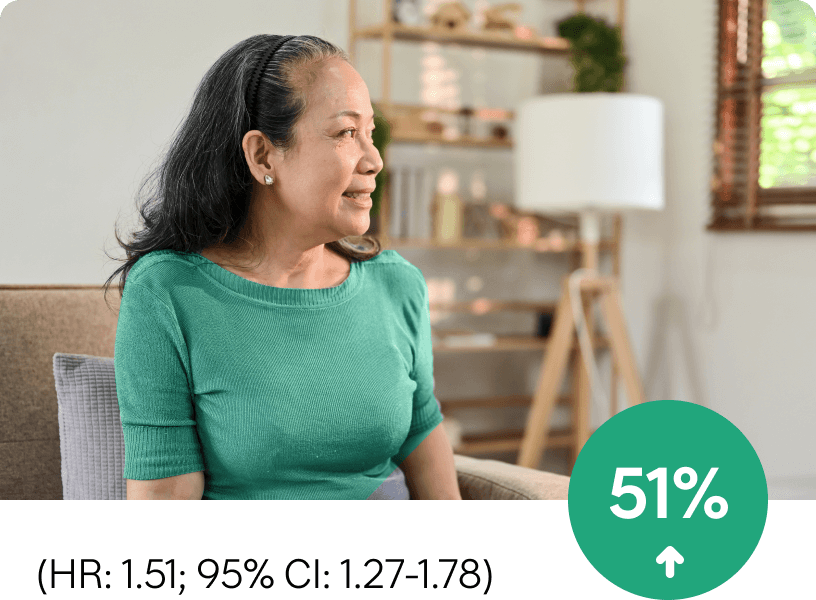
Compared with patients who did not receive KDE, receipt of KDE increased the likelihood of:
Receiving a kidney
transplant by
Being placed on a
kidney transplant waiting list
Being evaluated for a kidney
transplant by
In 2018, only ~1% of eligible patients with CKD stage 4 had a claim for kidney disease education10
Utilization of the CMS KDE benefit resulted in:
Increase in pre-ESRD wait-listing11,‡‡
Increase in PKT11,‡‡
Use of the Centers for Medicare and Medicaid (CMS) KDE benefit can help increase your PKT population.11
For appropriate patients:
Improve fragmented care7
CKD/End-Stage Renal Disease (ESRD) Patient journey2
Identifying and educating patients with CKD earlier can improve care and reduce barriers to transplant.12
Calculate your patient's Estimated Post Transplant Score (EPTS) to identify recipients who may
benefit most from rapid waiting list placement and transplantation.1
Candidates are less likely to lose their top-tier EPTS status when they are preemptively wait-listed.1

From 2015-2017, only 1 in 5 kidney
transplant candidates with top-tier EPTS
scores were preemptively wait-listed for
transplant.1

Candidates with a top 20% EPTS
status have preferential access to deceased
donor kidney offers with the lowest
cumulative risk factors.1
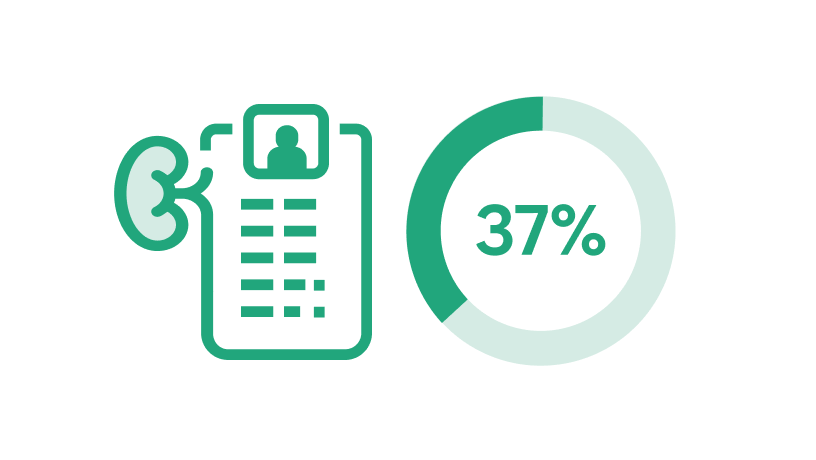
Only 37% of patients with top 20% ETPS
status were added to the waiting list within 3
years of dialysis initiation.1
For appropriate patients:
Improve health outcomes7
With a living donor, your kidney transplant candidates may achieve:
For appropriate patients:
Understand reimbursement of kidney transplants8
CMS reimbursement for kidney transplant admissions may vary depending on the assigned Medicare Severity Diagnosis Related Group (MS-DRG).8
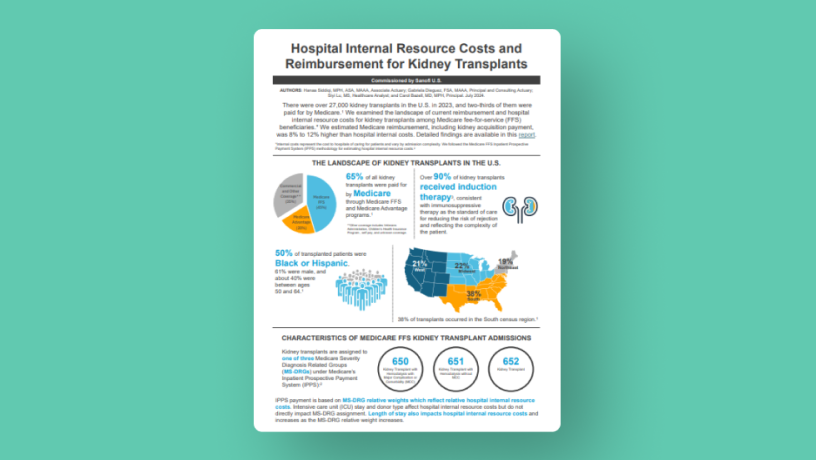
Kidney transplant admissions infographic
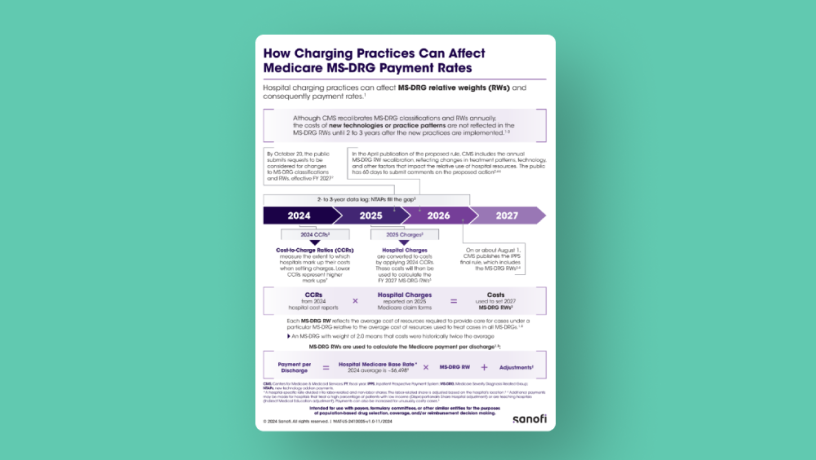
Medicare MS-DRG payment system
Stay up-to-date with professional guidelines5,14
Educate at CKD stage 4, refer at CKD stage 4, and transplant at CKD stage 514,##
The following guidelines assist health care professionals in the field of kidney transplantation to evaluate and manage care for their patients
To learn more, click on the individual guidelines below:
Resources to support your appropriate patients on the journey to
living donor PKT
The Advancing American Kidney Health (AAKH) Initiative aims to double the number of kidneys available for transplant by 2030, through strategies such as increasing available options for individuals in need of kidney transplants and access to PKT.7
Bring the experts in kidney transplant education to your patients! Click on each resource to learn more.

EXPLORE Transplant
Go to website

CMS Kidney Disease Education Benefit
Go to website
Kidney Failure Risk Equation
Go to website

EPTS Calculator
Go to website

American Society of Transplantation (AST) Living Donor Toolkit
Go to website
Living Donation Business Case Toolkit
Go to website
Work with kidney health management companies specializing in kidney transplants:
This listing is provided as a resource only and does not constitute an endorsement by Sanofi of any particular organization or its programming. Additional resources on this topic may be available and should be investigated. Sanofi does not review or control the content of non-Sanofi websites.
Learn about PKT and the Benefits of
Kidney Transplant
Strategies that align with the goals of the Increasing Organ Transplant
Access (IOTA) model
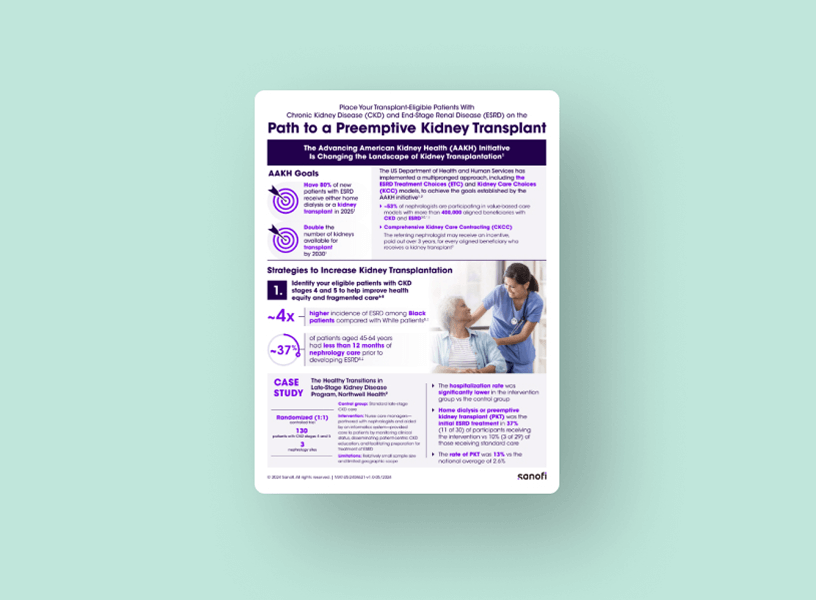
Path to PKT
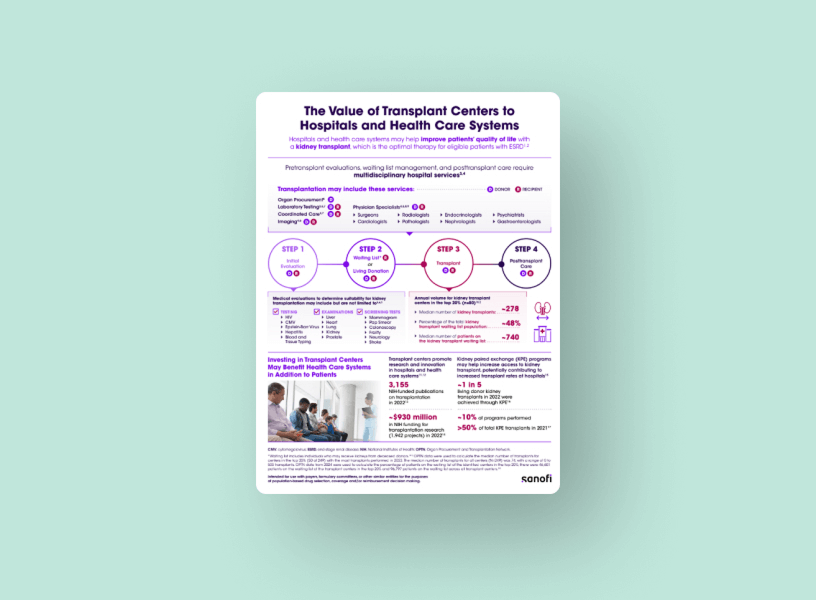
The Value of Transplant Centers to Hospitals and Health Care Systems
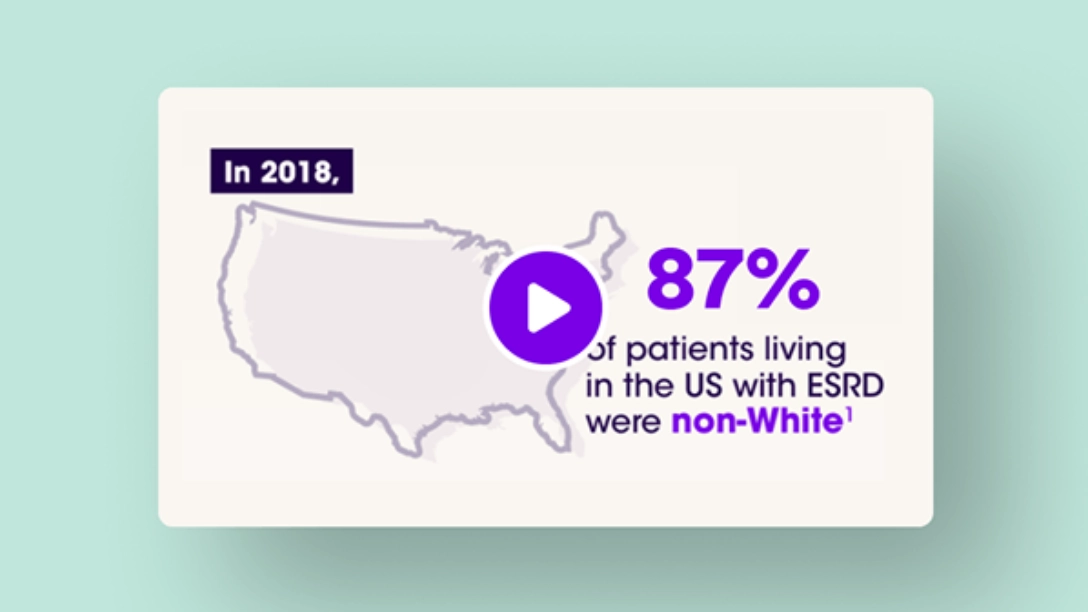
Learn more about the staggering disparities faced by those in need of kidney transplant
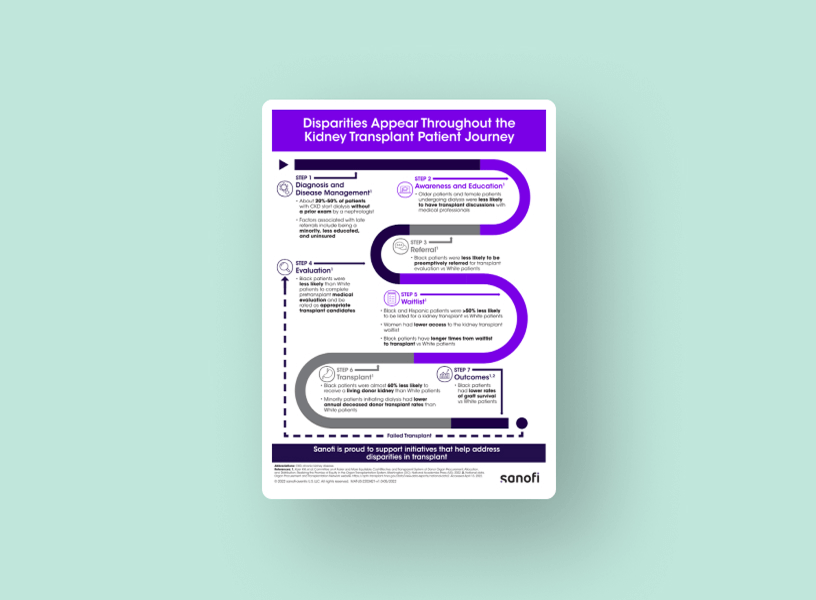
Disparities Appear Throughout the Kidney Transplant Patient Journey

Achieving Equity in Kidney Transplantation
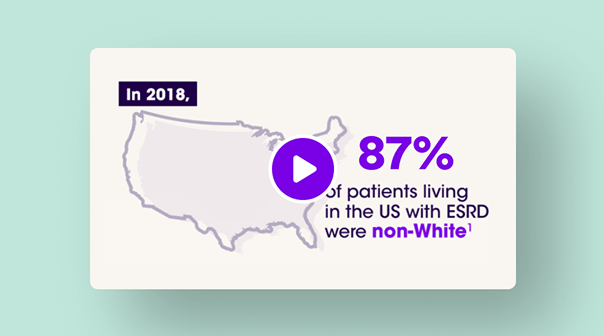
Disparities in Kidney Transplantation
Abbreviations, footnotes, and references
AAKH, Advancing American Kidney Health; AST, American Society of Transplantation; CKD, chronic kidney disease; CMS, Centers for Medicare and Medicaid Services; DD, deceased donor; EPTS, estimated post transplant score; ESRD, end-stage renal disease; FFS, fee for service; HD, hemodialysis; HR, hazard ratio; IOTA, Increasing Organ Transplant Access; KDE, kidney disease education; KDIGO, Kidney Disease Improving Global Outcomes; MS-DRG, Medicare Severity Diagnosis Related Group; OPTN, Organ Procurement & Transplantation Network; PD, peritoneal dialysis; PKT, preemptive kidney transplant; PPPY, per person per year; RRT, renal replacement therapy; USRDS, United States Renal Data System.
* Study included individuals ≥18 years of age (N=42,445) in the USRDS with top 20% EPTS scores. Patients had been preemptively waitlisted or had initiated dialysis between 2015-2017.1
† Incident cases of ESRD in 2022, USRDS.2
‡Data shows 1,994 LD procedures from a total of 4,949 preemptive kidney transplants = 40%. After dialysis population is 4,054 LD divided by 22,402 total transplants after dialysis (18%).3
§ Inflation-adjusted PPPY 2022.2
¶ Data shown are cumulative estimates. Based on a retrospective, observational cohort study using data on patients with ESRD from Optum Clinformatics Data Mart (2012-2021). All-cause medical and pharmacy costs were compared between patients who received PKT and those who received maintenance dialysis. Of patients who survived the 12-month follow up period, 1,530 received PKT and 14,763 received dialysis. Of patients who survived the 36-month follow up period, 551 received PKT and 6,199 received dialysis.9
# In 2022, there were 2,393 ESRD beneficiaries per 1 million lives (prevalence rate from USRDS ESRD database). Costs were based on the per person per year Medicare FFS spending for ESRD beneficiaries in 2022 ($99,369 for in center HD; $113,890 for home HD; $85,845 for peritoneal dialysis; $45,128 for transplant). The estimated cost per 1 million lives for dialysis was calculated using prevalence percentages of in-center HD (57.9%), home HD (1.6%), and peritoneal dialysis (8.3%). The calculated costs per 1 million lives for in-center HD, home HD, and peritoneal dialysis were then added to estimate the total dialysis cost per 1 million lives. For the hypothetical case, the prevalence percentage for dialysis was assumed to be 43% for in-center HD, 2% for home HD, and 5% for peritoneal dialysis, and the prevalence percentage for transplant was assumed to be 50%. The estimated annual savings was based on the difference between 2022 actual costs and a hypothetical plan, with savings calculated per 1 million lives.2
‖ Incident cases of ESRD in 2022, United States Renal Data System (USRDS) ESRD and OPTN waiting list history.2
** A group education session covering renal replacement therapy options (RRT) was conducted in adults aged >18 years with ESRD (n=80) in the Netherlands (2011-2013); RRT outcomes (date and type) up to 2 years post intervention were collected.6
†† Retrospective cohort study of patients aged ≥18 years used data from the Medicare-linked United States Renal Data System (2009-2019). Of all eligible patients with ESRD, 1.5% (7,838 of 519,902) received KDE; most patients (85.6%) had stage 4 CKD with comorbidities.9
‡‡ Based on 2013-2017 US data from adults aged ≥67 years who had CKD stage 4 (n=106,465); use of kidney disease education was examined in the 2 years prior to ESRD onset.11
§§ Based on prevalence of CKD in 2020.2
¶¶ Based on survival probability of living donor transplant vs hemodialysis reported for 2018.2
##CKD stage 4, estimated glomerular filtration rate (eGFR) 15-29 mL/min/1.73 m2; CKD stage 5, eGFR <15 mL/min/1.73 m2 or on dialysis.14
1. Schold JD, et al. J Am Soc Nephrol. 2021;32(7):1733-1746.
2. United States Renal Data System. 2024 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2024.
3. Lentine KL, et al. Am J Transplant. 2025;25(2,suppl 1):S22-S137.
4. Optum. Kidney Solutions: Preemptive Transplants Rates and Cost Savings. Eden Prairie, MN; Optum Inc; August 2021.
5. Chadban SJ, et al. Transplantation. 2020;104(4)(suppl 1):S11-S103.
6. Massey EK, et al. Nephrol Dial Transplant. 2016;31(5):823-830.
7. US Department of Health and Human Services. Advancing American kidney health. https://aspe.hhs.gov/sites/default/files/private/pdf/262046/ AdvancingAmericanKidneyHealth.pdf. Accessed February 4, 2025.
8. Healthcare Financial Management Association. Final rule summary: fiscal year 2021 Medicare hospital inpatient prospective payment system and longterm care hospital prospective payment system final rule. https://www.hfma.org/wp-content/uploads/2022/10/fy21-inpatient-prospective-paymentsystem-final-rule-summary.pdf. Accessed February 5, 2025.
9. Data on file. Sanofi; 2025.
10. United States Renal Data System. 2020 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2020.
11. Johansen KL, et al. J Am Soc Nephrol. 2020;31(suppl):18. Kidney Week abstract FR-OR11.
12. Helmick RA, et al. Transplant Direct. 2018;4(4):e356. doi:10.1097/TXD.0000000000000773.
13. Redfield RR, et al. Transpl Int. 2016;29(1):81-87.
14. Educational guidance on patient referral to kidney transplantation. Organ Procurement & Transplantation Network. https://optn.transplant.hrsa.gov/ professionals/by-topic/guidance/educational-guidance-on-patient-referral-to-kidney-transplantation/. Accessed February 5, 2025.




.png)
.png)